Robotic Prostate Cancer Surgery
Robotic Surgery
Robotic systems are becoming increasingly popular in the medical fraternity owing to the unique advantages including the precision, safety and many other advantages.
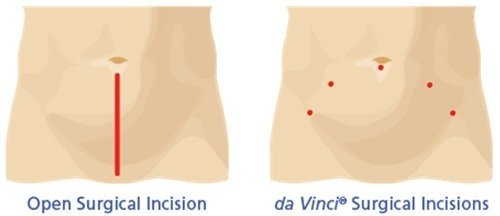
The da Vinci® robotic surgical system is one of the popular and widely employed robotic systems in the specialty of medicine and is used to perform surgical procedures in general surgeries and other specialties of medicine. The da Vinci® system offers a minimally invasive alternative option to traditional open and laparoscopic surgery. Most of the complex surgical procedures may be performed with the da Vinci® robotic system. Traditional open surgery uses a large incision and patients may experience complications such as pain, damage to the surrounding organs and nerves and long recovery period. In contrast, the da Vinci® robotic system is the most effective and least invasive technique which ensures faster recovery with minimal pain and minimal risks as compared with traditional open surgery.
The da Vinci® surgical system consists of a surgeon’s console, a patient-side cart with four interactive robotic arms, a high-performance vision system (3D camera) and miniaturised EndoWrist surgical instruments.
While performing the surgical procedure your surgeon will be seated at the da Vinci® console and is able to view a magnified, high-resolution 3D image of the area to be operated. To access the surgical site your surgeon introduces miniaturised EndoWrist instruments through few tiny incisions. These instruments help your surgeon perform the procedure with precision and control. Your surgeon uses master controls that function similar to forceps and in turn da Vinci® responds by immediate translation of surgeon’s directions into precise movements of miniaturised instruments.
The da Vinci® robotic system offers several advantages over the traditional surgery including less pain, low risk of infection, fewer complications, less scarring, less blood loss, short hospital stay and faster recovery.
The da Vinci® Robot System is considered safe and effective, but may not be appropriate for everyone. It is contraindicated in patients with bleeding disorders, history of previous surgery, pregnancy and cardiopulmonary diseases. Always discuss with your doctor about all treatment options suitable for you, as well as the benefits and risks.
What Is Prostate Cancer?
Around 20,000 Australian men are diagnosed with prostate cancer each year. It mostly affects men in older age groups and is rare in men under 45 years of age. The chance of developing prostate cancer is significantly higher in men who have a close relative with prostate cancer; the risks are higher if the relative was diagnosed before the age of 60.
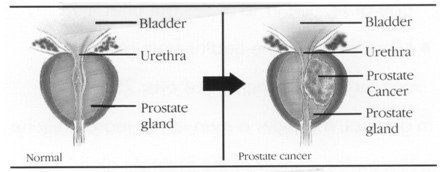
Prostate cancer is a disease in which malignant (cancer) cells form in the tissues of the prostate. The prostate is a gland in the male reproductive system located just below the bladder and in front of the rectum.
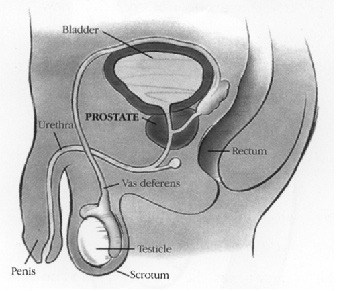
It is about the size of a walnut and surrounds the urethra (the tube that empties urine from the bladder- see picture below). The prostate gland produces fluid that is one of the components of semen.
Symptoms and Diagnosis
Urinary symptoms are nonspecific and include
- Frequent urination particularly at night
- Pain on urination
- Blood in the urine
- Weak stream of urine
Prostate cancer can spread to lymph nodes, bones (especially ribs and the hip and lower back), liver and lungs. When the disease spreads to the bones, it causes pain or unexplained weight loss and fatigue.
Diagnosis is made using a digital rectal examination to feel the prostate and a blood test for prostate specific antigen (PSA). The prostate gland makes PSA. It is a protein normally released into the blood by the prostate. The normal range of PSA in the blood is age specific. As a man gets older the PSA levels increase. The production of PSA is one of the functions of the normal, healthy prostate. This antigen is present in large amounts in semen and acts to prevent the semen from getting too thick.
A rectal ultrasound can image the prostate and multiple needle biopsies are used to detect the disease and determine its aggressiveness (the two most common Gleason grade of 1-5 pattern is added together to form a score; low scores of 5-6 indicate slow growing disease).
Treatments
Low-grade disease confined to the prostate may be ‘watched’ (called regular or active surveillance by doctor).
- Surgery can remove the whole prostate gland by either a conventional open radical prostatectomy or a robotically assisted radical prostatectomy.
- Radical radiotherapy can also be given with curative intent, either with external radiation or by implanting radioactive seeds (brachytherapy).
- For widespread disease, hormone therapy can be used. When hormone resistance occurs, chemotherapy can be used to control symptoms.
Robotic Assisted Radical Prostatectomy (RARP)
Robotic surgery is similar to laparoscopic or keyhole surgery. The surgeon operates through several small incisions.
The RARP is indicated for men with localised cancer of the prostate who have non-focal Gleason 6 and higher grade cancer. In high-risk prostate cancer cases, robotic-assisted extended pelvic lymph node dissection is also performed.
The surgery time can depend on a patient’s weight, the size of the prostate, the presence of scarring from previous prostate surgery or radiotherapy, and previous abdominal surgery. It usually takes between 2-3 hours to complete.
The daVinci Surgical System is the most commonly used robotic platform for RARP. The daVinci Prostatectomy is one of several minimally invasive surgical techniques that offer a safe alternative to open prostatectomy for removing the prostate.
Advantages
The daVinci Prostatectomy appears to have significant advantages over open prostatectomy in that it results in:
- Less bleeding and postoperative pain
- Shorter hospital stay
- Earlier return to work
More
Precise removal of cancerous tissue - Enhanced ability to perform nerve sparing surgery
- Lower risk of wound infection
- Fewer postoperative complications
- Less scarring
- Fewer days with a catheter
- Faster recovery of urinary and sexual function
After general anaesthesia is administered, the operation is performed through five to six small incisions across the middle of the abdomen. A pencil-sized binocular telescope held by one of the robotic arms is then inserted through an incision to provide X10 magnification, 3-D and high definition images of the surgical site (better than the human eye).
Fine robotic instruments are then inserted through other small incisions and are used to remove the prostate, seminal vesicles, and vas deferens while preserving the nerves for erectile function. Once the cancerous prostate gland is dissected free, it is placed into a small plastic bag, and eventually removed through one of the surgical incisions. Reconstruction is then carried out with the bladder sewn back to the urethra to restore continuity of the urinary tract.
A catheter is placed through the penis to drain the bladder and allow healing of the bladder-urethra connection. Once the prostate is removed, it is submitted to pathology for thorough evaluation to determine the Gleason grade, location, and extent of the cancer.

Potential Complications
Potential short and long term complications include:
- Bleeding
- Infection
- Urinary retention or incontinence
- Impotence, sterility
- Constipation
- Bladder spasms
- Anastomotic stricture
- Rectal injury
Preoperative Care
Attending the preadmission clinic is advisable. Here you will be informed about your operation and about your pre-operative and postoperative care. You will be required to have some blood and urine tests. An electrocardiogram will also be performed.
You will be taught how to do pelvic floor exercises that you will be required to do after your surgery and the removal of your catheter. It is advisable to practise these prior to your surgery.
You must cease any blood thinning medication such as aspirin, warfarin or plavix prior to your surgery. Your surgeon will advise you about this.
Ceasing fish oil, garlic, ginger and Ginko is also advisable as they have blood thinning properties.
You are to shower prior to your surgery with an antiseptic wash.
The day prior to your surgery you are to have a light diet during the day and in the evening to have clear fluids only. Some surgeons will require you to have a bowel preparation the night before surgery to empty the bowel. You are to be nil by mouth for six hours prior to your operation.
Hospital Stay
You will generally remain in hospital for one (1) or two (2) days and you will be able to return to work and perform full activities within 3–4 weeks after surgery.
Whilst you are healing you will have a catheter inserted into your bladder. The urine will be collected into a bag. You will be taught how to care for your catheter on discharge. The catheter will stay in for five (5) to seven (7) days after your surgery.
You will have intravenous fluids post operatively and you will have clear fluids for the first night. This will progress to free fluids and then a light diet the following day. There will be a drainage tube from your abdomen that will be removed on day one.
Most patients only feel slight discomfort around the lower abdomen. This is usually controlled with anti-inflammatory suppositories along with paracetamol. You may experience some shoulder tip pain as a result of insufflation of the abdomen with carbon dioxide (CO2) necessary to perform the surgery. Air sometimes can be trapped under the diaphragm. This will ease quickly and is helped by early ambulation. You are encouraged to drink about two (2) litres of fluid per day.
Discharge from Hospital
You will generally be discharged the following day or the second day after your procedure. Discharge time is generally between 9-10am. Please arrange for someone to collect you by this time. Before discharge your wounds will be checked and the dressings changed.
The first week post-operatively will likely be spent resting; however, frequent walks are encouraged. Depending on the individual, regular activities may resume as soon as a few days after surgery but straining and heavy lifting is discouraged for the first four weeks after surgery to promote internal healing. Normal bowel habits are sometimes disrupted after surgery. It is advisable to avoid constipation. Oral aperients can be given if necessary. Your nurse on discharge will advise if this is necessary. You will be educated on the care of your catheter that will be attached to your leg. Ensure the catheter is taped to your leg at all times.
You will have a follow up appointment with your surgeon. Not all surgeons perform a cystogram. A cystogram is an X-ray containing a dye to show that the bladder and the urethra have healed. If this has healed, you will have your catheter removed.
It is normal to have some urinary incontinence after the removal of the catheter. This can be for a short time or it can last up to 6- 9 months. The majority of men will become dry within the first four to ten weeks. Although a small number will have mild to moderate leakage that can last longer. It is very important to commence your pelvic floor exercises as soon as the catheter is removed.
You may experience some blood stained urine in the first couple of weeks after your surgery. However if bleeding becomes heavy, please contact your doctor.
Contact your doctor if you start to experience increasing pain or feel unwell, swelling or bleeding around your wound or if you feel the catheter is not draining well.
Effects of Treatments for Prostate Cancer
Incontinence
Surgery for prostate cancer can affect your bladder and the control of urination leading to incontinence. In a healthy urinary tract the bladder is able to collect and store a reasonable amount of urine before a person becomes aware of wanting to pass urine. There are two (2) sphincters which control the urine flow and these are both situated within the part of the urethra which is surrounded by the prostate. These two sphincters play an important role in keeping urine in the bladder and the conscious voluntary passing of urine. When an individual with a healthy urinary tract decides to pass urine, the bladder must contract and the sphincters relax so that urine is pushed out of the bladder. Following prostate surgery the bladder neck and the urethra take time to heal.
When your catheter is removed you can use the pelvic floor muscles to reduce or stop urinary leakage. Regular effective pelvic floor exercises will help defer an urge to urinate and improve bladder control. Mild to moderate urinary leakage can be contained in absorbent pads. A wide variety of pads are available in supermarkets and pharmacies. If incontinence is a long term problem financial assistance in obtaining pads can be obtained through Medicare and Centrelink.
Most people with incontinence use continence products such as pads or bedding protection to manage their condition. Some people require these products on a long term basis, which can become very expensive, and put unreasonable pressure on the household budget.
The Australian Government and State and Territory Governments offer a range of continence subsidy schemes to help offset some of these costs. These schemes have differing eligibility criteria and funding allocations.
Details of these subsidy schemes can be found by contacting a continence nurse advisor on the National Continence Helpline on 1800 33 00 66. The Helpline can also provide you product information and the details of local and national continence product suppliers.
The Continence Foundation recommends an assessment by a continence health professional to ensure that you or the person you are caring for uses the most appropriate continence product, including the correct fit and application of the product. To find out the details of your local continence professionalcontact the National Continence Helpline.
There are health professionals who are specifically trained to deal with incontinence. If you are concerned and wish to speak to someone, speak to your doctor or the incontinence hotline.
Pelvic Floor Exercises
What is your Pelvic Floor?
The floor of the pelvis is made up of layers of muscle and tissue. They are stretched like a hammock from the tailbone at the back to the pubic bone in the front. The pelvic floor supports the bladder and the bowel. The urethra and the rectum pass through the pelvic muscles. Like other muscles in the body we can control them. Exercise strengthens and improves muscle control.
Pelvic Floor Exercises
You can find many helpful resources to help with pelvic floor exercises. You will be given an extra handout. You can also download an app onto your phone or computer.
How can I find my pelvic floor muscles?
The first step in performing pelvic floor muscle exercises is to identify the correct muscles. There are several ways to identify them.
Method 1 – Stopping the flow
When you go to the toilet, try to stop or slow the flow of urine midway through emptying your bladder. If you are able to do this you are squeezing the correct muscles. Do not do this repetitively. This is not an exercise, but a way to identify the correct muscles.
Method 2 – Visualization
Stand in front of the mirror (with no clothes on) and tighten your pelvic floor muscles. If you are tightening the right muscles, you should see the base of the penis draw in and scrotum lift up. The back passage will tighten too but it is not the focus of the exercise. When you relax your muscles, you should feel a sensation of ‘letting go’.
Getting the technique right
Correct technique is very important when doing pelvic floor muscle exercises. You should feel a ‘lift and a squeeze’ inside your pelvis. The lower abdomen may flatten slightly, but try to keep everything above the belly button relaxed and breathe normally. A continence physiotherapist, continence nurse advisor or urology nurse can help if you have trouble identifying your pelvic floor muscles.
Exercising your pelvic floor muscles
Once you master the art of contracting your pelvic floor muscles, try holding the inward squeeze for longer (up to 10 seconds) before relaxing. If you feel comfortable doing this, repeat it up to 10 times. This can be done three times a day. Make sure you continue to breathe normally while you squeeze in. You can do the exercise lying down, sitting or standing with your legs apart, but make sure your thighs, bottom and stomach muscles are relaxed.
Many men find it difficult to remember to do their pelvic floor exercises. Linking the exercises to a regular activity such as meal times or brushing your teeth is a good way to incorporate them into your daily routine.
Important information
Performing pelvic floor muscle exercises after prostate surgery is vital to your recovery as it is these muscles that help you control your bladder. Doing pelvic floor muscle exercises after surgery (whilst a urinary catheter is in place) can irritate the bladder and cause discomfort. It is therefore recommended that you do not do any exercises during this time. However, once the catheter is removed you may start the pelvic floor exercises straight away.
Impotence
Your surgery can cause impotence firstly due to the damage to the nerve bundle running past the prostate to the penis and secondly, by interrupting the blood supply to the penis during surgery. Your surgeon will always endeavour to minimise any damage to the nerves during surgery. Your ability to obtain an erection following your surgery will be effected by your ability prior to surgery and your age. However, things may improve with time. The early use of chemical or mechanical devices to obtain an erection after your surgery, in many cases can help return you to normal erectile function. In addition, you will notice changes to ejaculation after surgery. Most patients will experience a dry orgasm. Some may experience the passage of urine during orgasm, known as climacturia. If this occurs, speak to your surgeon.
Some men are unconcerned about their impotence. However there are some options for those who wish to do something about it. It is important to add that these treatments need a certain amount of practice to get them right.
Medications
A tablet such as sildenafil (Viagra) can help some men achieve an erection or a stronger erection. Viagra does not increase your sex drive and does have some side effects. Research has shown that Viagra only works on some men. It is important to discuss with your doctor any other medications you are on before taking Viagra.
Injections can be given directly into the penis and they are the most effective form of treatment to achieve erections following a prostatectomy. This drug needs to be injected each time an erection is required. It is important to discuss this option with your doctor. He will prescribe the correct dosage. One of the side effects is a prolonged and painful erection that will require urgent medical intervention. There is some evidence that by using the injection to keep your penis working after the surgery, you may recover your own ability to achieve erections more quickly.
Devices
A vacuum erection device is a pump that is placed over the penis and a vacuum is created to draw blood into the cavities. Once the penis is erect a ring is placed around the base of the penis and the pump is removed. When the erection is no longer needed the ring is removed. This option requires a certain amount of manual dexterity.
If all the above options fail to achieve an adequate erection, a penile prosthesis can be placed within the penis to create an artificial erection.
It is possible to use a variety of options to manage impotence. Many men use a mixture of treatments such as an injection on one occasion and then focus on other aspects of sexual activity on the rest of the time. Many sexual activities can be done with a limp or semi-rigid penis. As long as you are aroused, you can enjoy a satisfactory sex life. Stimulation can be enhanced using a lubricant or can be done manually, orally or with a vibrator.
It is important to involve and communicate with your partner. Sex is an important part of most couples relationships’ and it is worth breaking the ice and sharing your concerns and worries with each other. It can be difficult to share this with each other. You may feel embarrassed or ashamed about talking about sexual health. There is no need to be. If you have any concerns, speak to your doctor and he can refer you to the appropriate professional.
Follow up Care
After treatment for prostate cancer, your doctor will monitor you carefully, checking your PSA to see if cancer returns. The doctor should also outline a follow-up plan. This plan usually includes regular doctor visits, PSA blood tests and digital rectal exams.
References
- Cancer Council Australia. www.cancercouncil.com accessed March 2014
- www.davincisurgery.com accessed March 2014
- www.prostate.org.au accessed March 2014
- www.continence.org.au accessed March 2014
- www.pelvicfloorfirst.org.au accessed March 2014
- Buckley,L. Cinahl Information Systems Aug 2012 Prostatectomy, Radical, Robot assisted, laparoscopic
- Starnes,D. Simms,T. Urological Nursing Vol 26 No.2 April 2006. Care of the patient undergoing robotic-assisted prostatectomy
- Continence Foundation of Australia 2012 Prostate, Continence and Prostate. A guide for men undergoing prostate surgery
Helplines
| National Continence Helpline | 1800 33 00 66 |
| Prostate Cancer Foundation of Australia | 1800 22 00 99 |
| The Cancer Helpline | 13 11 20 |
| Australian Physiotherapy Association | (03) 9534 9400 |